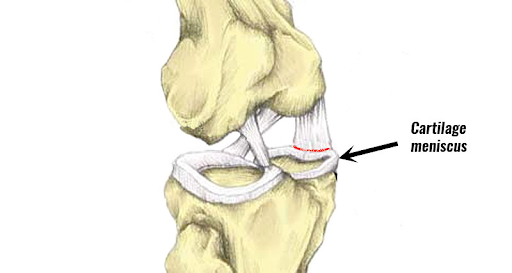
It sits on the tibial plateau (top surface of the shin bone) between the tibia (shin bone) and the femur (thigh bone).
They are important for distributing load and absorbing shock at the knee joint.
There are two menisci within each knee joint and they are ‘C’ shaped discs, made of tough cartilage called fibrocartilage.
How do meniscal tears occur?
Meniscal tears can be degenerative or traumatic and it can occur in a number of ways. It can happen on its own or in combination with a ligamentous injury.
The most common cause is usually damaged by a twist occurring on a slightly bent position of the knee.
A partial or total tear of a meniscus may occur when a person quickly twists or rotates the upper leg while the foot stays planted.
Degenerative tears occur as part of progressive wear in the whole joint or as a result of habitual, prolonged squatting. In the older adult, the tear may be due to a natural degeneration of the menisci that occurs with age. The medial meniscus is more commonly affected than the lateral meniscus, whilst tears in both menisci are much less common.
Can a meniscus tear heal on its own?
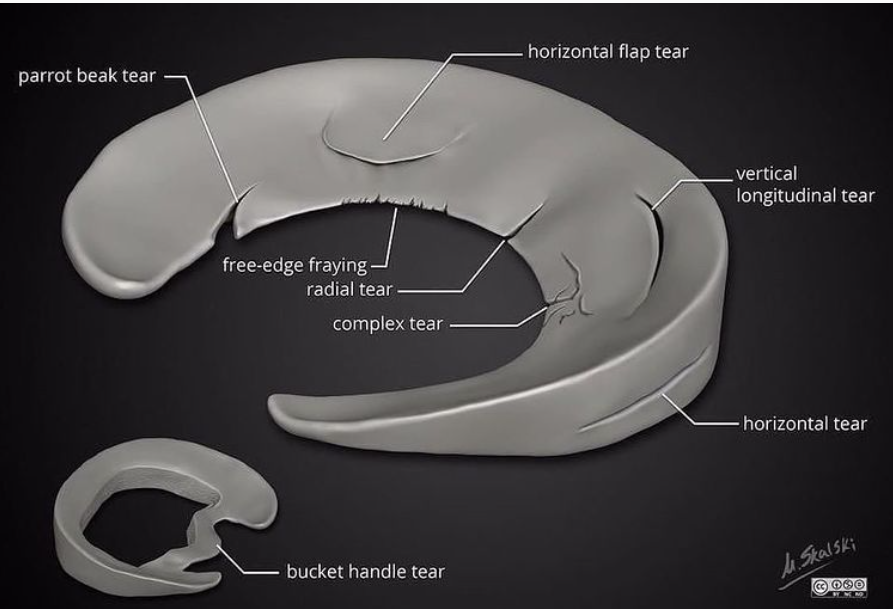
This will all depend on the type of tear that occurs and the location of the tear.
If your tear is on the outer one-third of the meniscus, it may heal on its own or with a small surgery. A longitudinal tear is an example of this kind of tear. Conservative is usually the better choice. This is because this area has a rich blood supply and blood cells can regenerate meniscus tissue.
Overall there is a higher chance the meniscal tear will repair on its own if the location is outer third and also small meniscal tears (less than 5mm) have the potential to heal on their own.
However if the tear is in the inner two-thirds, which lacks blood flow, the tear most of the time cannot be repaired and may need to be trimmed or removed surgically. Like a complex tear or radial tear.
There is some research that suggests trying conservative measures first by strengthening the hip girdle and muscles around the knee and improving movement patterns, then re-assessing. Once again it will depend on how much your function is limited and if there is continuous locking and giving way during daily activities.
For the inner two-thirds surgery is typically the best course of treatment as mentioned. The goal of surgery is to preserve the meniscus by repairing or removing the torn part. The procedure is typically done arthroscopically, meaning a small camera is inserted into a tiny incision in the knee to guide the surgeon in repairing or removing the tear using small instruments inserted into another tiny incision.

How do you check yourself for a torn meniscus?
Initially, there are typical signs to indicate some type of injury is present. Like with most soft tissue injuries; swelling, stiffness and pain are usually an indicator of something gone wrong. Though this may not specify the exact issue within the site it may prompt you to investigate further.
A torn meniscus would typically manifest with swelling and tenderness around the inner and outer knee joint lines with or without limited or painful knee active range of movement.
Considering these structures are injured due to rotational forces, the Thessaly’s test would be fitting to reproduce your symptoms. Though, be mindful that this test can really stir up your pain.

Begin by standing on your affected leg with a slight bend at the knee. While maintaining this stance, slowly turn your body all the way left then right while maintaining a planted foot. A positive sign is a reproduction of your pain on rotation.
This would merit a visit to your local physiotherapist for a thorough examination to determine the extent of your injury or if further imaging is required. Following this, a strategy will be developed to address the contributing factors of your injury which may address stability or mobility training of the joints above or below to prevent symptom relapse.
What Can Mimic A Meniscus Tear?
According to Barker and colleagues, common extra-articular pathologies that can mimic lateral meniscal tears include iliotibial band syndrome, proximal tibiofibular joint instability, snapping biceps femoris or popliteus tendons, and peroneal nerve compression syndrome or neuritis (Barker, Strauss, Lodha & Bach, 2010). Other notable structures are the lateral collateral ligament and the posterior cruciate ligament.
For more medial structures, this can be due to injury to the medial collateral ligament, the pes anserine bursa or symptoms due to patellofemoral joint syndromes.
A visit to your local physiotherapist would be helpful to determine the exact injured structure. This may include further scans to confirm diagnosis or rule out any further pathology.
#MakingHeathySimple
Aarvi & Mike
